Rheumatoid arthritis affects about 1% of people around the world. About 1.3 million people in the U.S. have it, with more than twice as many of those being women [1]. However, there are over 32 million people in the U.S. who have osteoarthritis. Why all the differences? Is rheumatoid arthritis genetic? There are a number of genes involved in inflammation and immune function, two major components of RA. Let’s dig into things a little deeper.
Introduction To Rheumatoid Arthritis And Genetics
To be very clear, there is a great deal of difference between the types of arthritis. The term itself means, “disease of the joints,” and there have been over 100 various forms of it described by medical professionals [2]. That said, there are two broad categories that seem to define the major differences, which are inflammatory and non-inflammatory. This is due to the causes of the arthritis.
Rheumatoid arthritis is actually one of a number of rheumatic diseases, many of which have nothing to do with joints. They can affect muscles, tendons, organs, and are generally considered musculoskeletal in nature [3]. It’s an autoimmune disease, where your immune system mistakenly reacts to healthy cells as foreign invaders, causing all kinds of potential problems [4]. This causes inflammation, tissue damage, and pain [5].
Compare this to the most common form of arthritis, osteoarthritis, which is commonly due to degeneration of the bone, and is what is typically thought of when the condition is arthritis. So, be wary, when someone says they have arthritis, that this could mean a wide variety of things.
When the disease is in the joints, rheumatoid arthritis usually affects the hands and feet, specifically the lining of the joints. Its signs and symptoms include [6, 7]:
- Joint pain and tenderness
- Heat and swelling in the affected joints
- Joint stiffness
Many people have periods of worsening symptoms called “flares.” These flares may be triggered by stress, too much movement, or a change in medication [8].
One important risk factor when it comes to rheumatoid arthritis is genetics. Genes involved in this condition may influence [5, 9]:
What Does Rheumatoid Arthritis Feel Like?
Arthritis can be everything from a nuisance to downright debilitating. It’s typically thought of as a condition of older people, but statistics show that it can even happen to children.
It’s often shrugged off as something you “just deal with”. Stiff joints and pain when you get up in the morning are just natural things that happen as you get old. We point out these cliches because, in reality, it can often be much more than that.
But what does rheumatoid arthritis feel like?
Medical terminology tends to be devoid of emotional language. It works in the realm of plain, dry facts, which is done for a reason. Experiences and responses vary widely across individuals. In light of that and to provide a hopefully more realistic idea of this condition, here is a comparison of medical description versus personal experience [6, 10]:
- Tender, warm, swollen joints VS. Burning, throbbing, gnawing, aching joint pain all while someone has your extremities in a vice trying to turn and twist them into a new direction
- Joint stiffness that is usually worse in the mornings and after inactivity VS. Feeling like the Tin Man from The Wizard of Oz with how stiff I consistently feel
- Fatigue VS. Overwhelming debilitating exhaustion that feels like a concrete wall stopping you from completing the simplest tasks
- Fever VS. A constant nagging flu
Perhaps the most telling and the best generalized feeling is this, “While I am only 34, I feel like I am 87 and have more in common with senior citizens than most people my age.”
But if it’s not a condition of the old, what affects rheumatoid arthritis? Genetics is involved, and we’ll discuss this below.
Can Rheumatoid Arthritis Be Reversed?
There currently is no cure for rheumatoid arthritis, but a lot of research has been done in the past couple of decades trying to gain a better understanding of what causes these autoimmune reactions by the body. One promising example is in examining the links between the gut microbiota and immune response [11].
Instead, patients and doctors work to control symptoms and manage pain. Some ways to manage the condition include [12, 13]:
- Medications
- Surgery (e.g., joint replacement surgery)
- Exercise
- Supplements to reduce inflammation and support bone health
While rheumatoid arthritis can’t be reversed, it is possible to reduce symptoms to manageable levels or even have it go into remission.
What Are The Risk Factors For RA?
We don’t fully understand the causes of autoimmune joint inflammation. Environmental factors such as nutrition and exposure to infections early in life may impact your risk [14, 15]. The exact cause likely differs across individuals. Other risk factors include [14, 5, 6]:
- Cigarette smoking
- Obesity
- Gender (females are more likely to get RA)
- Age (risk increases with age)
- Gum disease
- Genetics
The Genetics Of Rheumatoid Arthritis
So, how is rheumatoid arthritis genetic? When you are talking about conditions related to your immune system, it’s almost a guarantee that your genetics will have an impact on it, whether it’s for the risk of getting the condition, its severity, or the ability to manage symptoms. This is to say that the risks of RA are hereditary.
Up to 65% of differences in people’s chances of developing rheumatoid arthritis may be attributed to genetics. Since RA is an autoimmune disease and involves inflammation, genes related to these factors are going to feature most prominently. The most likely possibilities include HLA-DRB1, STAT4, and IL10 [5, 9].
The HLA-DRB1 gene codes for a receptor on our white blood cells, which helps with determining what cells are bad and need removing. A variant in this gene can make it more likely that good cells will be viewed as invaders and it likely increases joint inflammation.
Another important gene is STAT4, which encodes a protein that helps activate the immune system and create T-cells to help fight “invaders”. A variant in this gene can result in increased immune response.
Lastly, we have IL10, or interleukin 10. If you do much digging around about the immune system, you will see interleukin involved in all sorts of ways. It can have both positive and negative effects, depending on the context. In this case, IL10 decreases inflammation, so a variant that lowers IL10 levels can make it more difficult for the body to control an inflammatory response.
Analyzing Your DNA Can Help You With RA
All of this is not to say you’re doomed depending on your genetics. Rheumatoid arthritis is manageable, and having your DNA analyzed can help you understand what risk factors are relevant to you based on your genes and what you can do to address them.
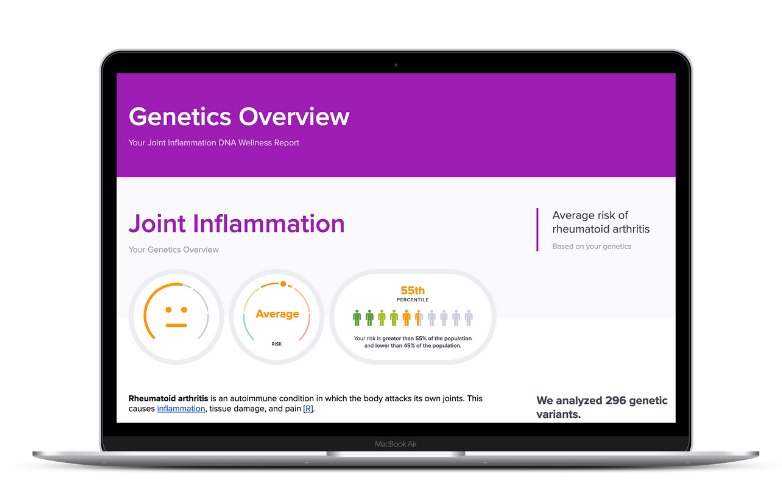
The SelfDecode Joint Inflammation Report allows you to optimize your health by uncovering what your genes are doing behind the scenes to affect your odds of struggling with joint inflammation.
SelfDecode analyzes nearly 300 genetic variants related to joint inflammation to give you the most precise data on your personalized report.
SelfDecode calculates your genetic risk for joint inflammation and provides evidence-based diet, supplement, and lifestyle recommendations to help you optimize your actions.
For example, you may be able to target inflammation by identifying whether you carry risk variants of genes such as TNF or CRP. People with these variants may benefit from getting more omega-3 fatty acids or maintaining a health weight, respectively [5, 16, 17, 18].
When you sign up for SelfDecode, you’ll gain access to over 30 DNA wellness reports covering a variety of health topics, including joint inflammation, joint pain, and bone health.
Concluding Remarks About Rheumatoid Arthritis And Genetics
RA can be a brutal condition. It is not your typical arthritis. It can require diligence and adherence to strict regimens to keep it under control. Understanding how your genetics can influence your body’s reactions to things can help form the groundwork for taking positive steps to address RA.
But knowing whether rheumatoid arthritis is genetic is just the beginning. Your DNA can help you discover which strategies may work best to help you improve your overall wellbeing.
Be proactive and start today by investigating your DNA to discover more about your health. For a gene-based approach to joint inflammation, you should check out SelfDecode.