Osteoarthritis (OA) is the most common form of arthritis, often termed “wear and tear” arthritis. It’s a condition caused by overuse, but this notion is limiting to what the condition is and how to deal with it. Is osteoarthritis genetic? Yes, genetics definitely plays a role, and we’ll see how below.
Osteoarthritis vs Rheumatoid Arthritis
A note first about rheumatoid arthritis (RA). It has, is, and can be fairly easily confused with osteoarthritis. If someone told you they had arthritis in their hands or knees or any other joint, you would have no way of knowing, just by looking at them, what kind of arthritis they had.
They both involve pain and inflammation in the joints. They can both be debilitating to the point of needing assistance for particular activities. So, what’s the difference between osteoarthritis and rheumatoid arthritis?
Osteoarthritis involves the breakdown of cartilage, that cushion material between the bones in the joint. RA, on the other hand, is an immune system disorder that causes tissue in your joint to be attacked [1].
Why is it important to distinguish the two? Well, because they have different causes, which changes not only how you go about preventing and treating the symptoms, but what genes might be involved as well. But are rheumatoid arthritis and osteoarthritis genetic? Yes, they have a genetic component. For example, you will find gene variants for the immune system with RA, but with OA you can see variants for bone strength and formation.
Some Facts About Osteoarthritis
Osteoarthritis is a complicated disease, and it doesn’t just come from “wear and tear.” If you thought it was a condition of the old, well, you would be correct to a point. The highest incident rate of OA is in the oldest age range. But don’t think you’re safe just because you’re young. There is still a noticeable chance of getting it even in your 20’s [2].
The biggest factor that can affect your risks for joint issues at a younger age? Weight. The past few decades have seen a continual growth in the number of people gaining enough weight to be classified as obese. So, there’s good reason why OA affects over 32.5 million US adults.[3].
What is Osteoarthritis?
A joint is any place where two or more bones meet. Each joint has layers of protective cartilage that help it move smoothly. In osteoarthritis (one of several forms of arthritis), cartilage breaks down, causing pain. Sometimes, the bone can thicken or grow in harmful ways [4].
Osteoarthritis tends to affect knees, hands, and hips. People with this condition may experience [4, 5]:
- Joint pain and stiffness
- Difficulty moving
- Weakness and balance problems
- Inflammation
- Popping, cracking, or grinding sensations in the joint
The cartilage is made up of a specialized network of various proteins, made and controlled by special cells called chondrocytes. When these cells start to fail via atrophy or imbalances in the system, OA can occur [6].
Cartilage has poor regenerative capability, which is why once OA sets in, it can’t really be gotten rid of, and it then becomes symptom management.
For this reason, the goal should be to prevent this kind of atrophy or imbalance from happening. The first step in that is knowing the risk factors for osteoarthritis. Genetics is involved, but there are also other elements that can also play a role.
What Are The Risk Factors For Osteoarthritis?
Most people with osteoarthritis are over the age of 55. In fact, older age is the number one risk factor for this condition. Other risk factors include [3, 7]:
- Being a woman (estrogen is a factor)
- Joint injury or overuse
- Obesity
- Bone deformities
- Diabetes
- Genetics
Women get the short end of the stick with this disease, as it seems estrogen has an effect on cartilage, which is why overweight women over 55 have the highest risk for OA [8].
The Genetics Of Osteoarthritis
Is osteoarthritis genetic? Well, about 50% of the differences in people’s chances of getting osteoarthritis can be attributed to genetics. Genes that contribute to osteoarthritis may influence [9, 10, 11]:
- Collagen production in the joints (COL2A1, COL11A1, and COL1A1)
- Inflammation (IL1B, IL4R, IL17A, IL17F and IL6)
- Activity of joint cells (ESR1)
- Bone formation (FRZB, VDR)
- Bone strength (IGF1, TGFB1, TIMP3, and ADAM12)
We’ll focus on collagen because it’s the element most within your control to do something about. Collagen is a structural protein, used throughout the body for a variety of purposes. There are 28 different types of collagen, encoded by 43 different genes [12]. This makes for a lot of potential changes due to genetic mutations.
With regard to OA, there have been family studies showing that a type 2 collagen gene polymorphism in COL2A1 is a strong hereditary factor [13]. This is the type of collagen in the cartilage between the joints.
Collagen happens to be one of those things you can supplement with, though it’s more effective for some than others, which can be influenced by genetics. In addition, there are other types of supplements that can help your body make more collagen, such as avocado-soybean unsaponifiables.
While you might be able to offset collagen loss, it doesn’t really mitigate issues like weight, diabetes, or excessive use of your joints, which can significantly affect your risks for OA. So, always remember to keep general, optimal health in mind, as it will help you in the long run.
How Can Analyzing Your DNA Help You With Osteoarthritis?
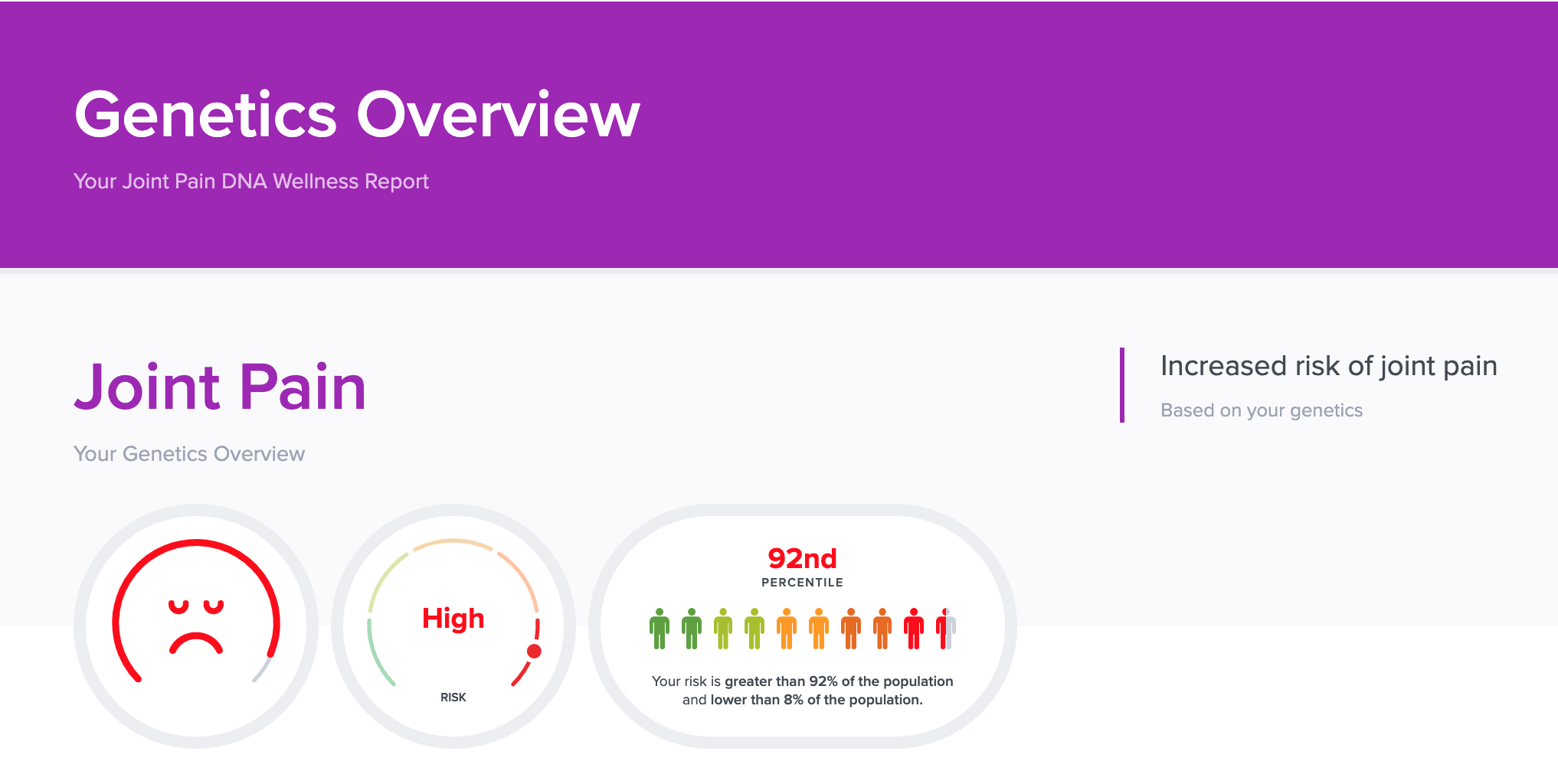
Now that you know more about osteoarthritis and genetics, you may be wondering how this can help you. Having your DNA analyzed can help you understand what risk factors are relevant to you based on your genes and what you can do to address them.
Not only can your DNA affect your risks for joint issues, but it can also influence how well you respond to wellness strategies to help manage your pain. The SelfDecode Joint Pain report allows you to optimize your health by uncovering what your genes are doing behind the scenes to affect your joint health.
One of those behind the scenes genes that you wouldn’t necessarily consider, at least until you were older, is the ESR1 gene. Loss of estrogen as women get older can significantly increase your OA risk already, but there are mutations in this gene that can either increase or inhibit this risk [11]. Having this information can better inform your health decisions.
By knowing your genetic predispositions, you can make targeted changes to your lifestyle to counteract the negative effects of your genes. Is osteoarthritis genetic? Yes, it can have a genetic component, but there are steps you can take to address your risks.
For example, if you have a certain COL2A1 gene variant, supplementing with collagen or avocado-soybean unsaponifiables may be more effective for you. On the other hand, if you have a variant in the HBL-DPB1 gene, curcumin may help you soothe your joint pain by reducing inflammation [14, 15, 16, 17].
SelfDecode analyzes over 385,000 genetic variants related to joint pain to give you the most precise data on your personalized report.
Unlike other DNA companies, SelfDecode goes a step beyond merely highlighting your genetic risk for joint pain. Your report also comes with evidence-based diet, supplement, and lifestyle recommendations to help you optimize your joint health.
Concluding Remarks About Osteoarthritis And Genetics
If you do nothing about it, arthritis is one of those things that you are inevitably bound to have to deal with. With each passing decade, the risks go up, particularly if you’re a woman. There are other risk factors involved with osteoarthritis, genetics included, but knowing where you stand can give you an advantage when it comes to optimizing your joint health.
While it is very easy to have an, “out of sight, out of mind” attitude about it, taking steps to mitigate the risks and effects earlier in life can help save you from a lot of pain down the road.
Be proactive and start today by investigating your DNA to discover how genetics can affect osteoarthritis. For a gene-based approach to joint health, you should check out SelfDecode.
Related Articles
- Is Rheumatoid Arthritis Genetic? Can Genes Affect Risk For Joint Pain?
- Is Obesity Genetic? Risk Factors & What You Need To Know