In recent years, genetic testing has moved into the spotlight as a tool people use to understand their health and make better lifestyle decisions. Many companies promise insights into disease risk and wellness based on your DNA.
The catch is that a lot of consumer DNA reports focus on single nucleotide polymorphisms, or SNPs, and highlight just a few “important” variants. They make it seem like knowing one or two genes gives a clear picture of disease risk. That’s a major oversimplification.
This article explains why advanced Polygenic Risk Scores (PRS) are far more reliable. By analyzing thousands or even millions of variants together, PRS captures the complexity of genetic influence on health, offering a much clearer view of risk and actionable insights.
To see PRS in action, platforms like SelfDecode and PromicsEdge, powered by OmicsEdge, give both consumers and professionals access to advanced risk prediction.
Understanding the Basics: SNP Analysis vs. PRS
Your DNA contains millions of small variations, among which are single-nucleotide polymorphisms, or SNPs. These are small differences in your genetic code, and certain SNPs have been associated with slightly increased or decreased risks for specific health conditions.
Most consumer DNA companies rely on a handful of SNPs to make predictions, highlighting only the so-called “significant” variants. The limitation of this approach is clear: each individual SNP typically contributes less than 1% to the overall risk of a complex condition.
Evaluating only a handful of variants provides an incomplete view, akin to attempting to understand an entire book by reading a single sentence. While these tests can generate interesting insights or headlines, they lack the depth necessary to guide meaningful health decisions.
One reason this approach persists is cost and simplicity. Developing a predictive model that incorporates thousands or millions of genetic variants requires substantial investment, expertise, and time. Many companies rely on limited SNP analysis because it is far less expensive and easier to market, even though it significantly reduces predictive accuracy.
This is why OmicsEdge provides advanced PRS as a service, helping health-tech companies integrate validated, accurate risk prediction into their products rather than relying on outdated single-SNP testing.
Polygenic Risk Scores (PRS) offer a more sophisticated alternative. PRS integrates the effects of thousands to millions of SNPs into a single, weighted score that reflects an individual’s overall genetic risk. By capturing the polygenic nature of most diseases, PRS provides a more comprehensive and accurate assessment of health risk.
This approach allows for evidence-based risk assessment and supports more informed health and lifestyle decisions. In contrast to single-SNP analysis, PRS provides actionable, science-driven insights that offer a clear view of both potential vulnerabilities and areas of strength.
The Cost and Complexity of Building an Advanced PRS
Developing a truly advanced Polygenic Risk Score is not simple or cheap. A basic SNP-based panel, often marketed by consumer genetics companies, can be built for just a few thousand dollars. It’s relatively quick to assemble and doesn’t require deep expertise in statistical genetics or large-scale data modeling.
In contrast, building a high-performing PRS that analyzes thousands to millions of SNPs requires substantial investment, access to large genetic datasets, and a specialized team of geneticists, bioinformaticians, and data scientists. For example, our OmicsEdge PRS platform took approximately $25 million and years of development to reach its current level of performance and validation.
It’s no surprise that many companies stick with single SNPs or a small set of “significant” GWAS hits, as they are dramatically cheaper to produce and easier to market to a general audience. Unfortunately, this cost-saving approach comes at the expense of accuracy and scientific validity. The truth is that building a robust PRS is resource-intensive precisely because it’s designed to reflect the true complexity of human disease.
OmicsEdge addresses this by offering custom PRS solutions for health-tech and biotech companies, ensuring they can deliver accurate, validated predictions to their users.
How Predictive Accuracy Is Measured: Understanding AUC
Predictive models are only as valuable as their ability to distinguish between individuals who will develop a condition and those who will not.
The most widely used metric for measuring this performance is the Area Under the Curve (AUC), derived from the Receiver Operating Characteristic (ROC) curve, which plots the true positive rate (how well we identify those with a condition) against the false positive rate (how often we incorrectly flag those without it) across different thresholds.
The AUC value, shown as a percentage, tells us how effectively a model or test distinguishes between two groups: individuals with and without a specific disease.
In practical terms, an AUC of 50–60% indicates poor discrimination, barely better than chance. Models in this range cannot reliably separate affected and unaffected individuals and have minimal clinical utility.
AUCs between 60–70% are considered fair, showing some ability to distinguish risk but remaining limited. These models may be useful as supplementary tools but are not dependable as standalone predictors.
AUCs of 70–80% indicate good discrimination, which is typically sufficient for clinical applications when paired with additional assessments. Models achieving 80–90% are considered very good, offering fewer errors and higher reliability.
Finally, AUCs above 90% are rare and represent excellent discrimination. Reaching this level is difficult due to biological and clinical complexities, but models in this range are highly reliable for risk prediction.
These simpler models typically produce AUCs below 70%, meaning their predictive power is limited. In contrast, advanced PRS models are able to achieve much higher AUCs, reflecting their ability to capture the polygenic nature of most diseases.
Comparing Models Across Diseases
OmicsEdge has created an advanced Polygenic Risk Score (PRS) that looks at many more genetic variants than usual. By also including clinical and demographic factors, it gives more accurate and reliable predictions than traditional methods.
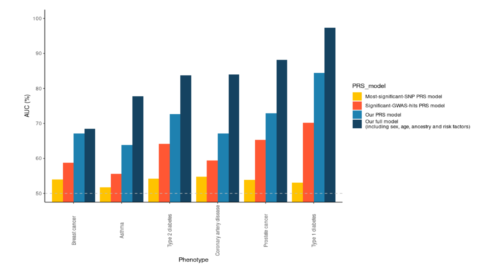
To evaluate the effectiveness of different genetic risk models, four approaches were compared across six common disease phenotypes: breast cancer, asthma, type 2 diabetes, coronary artery disease, prostate cancer, and type 1 diabetes. The models assessed include:
- Most significant-SNP PRS model: Uses only the single most significant genetic variant.
- Significant-GWAS-hits PRS model: Relies on a handful of GWAS-identified variants.
- OmicsEdge PRS model: Incorporates a broader range of genetic data to capture more of the polygenic signal.
- OmicsEdge full model: Combines genetic information with additional factors such as sex, age, ancestry, and other risk indicators, as implemented in the Longevity Screener.
As shown in the graph below, the difference in accuracy between these models is striking.
The validation set results from these models highlight clear differences in predictive performance.
The Most Significant SNP PRS Model generally shows AUCs between 50% and 60%, barely above random chance. This reflects the limitation of using a single genetic variant, which captures only a minimal fraction of overall disease risk.
The Significant-GWAS-hits PRS model performs slightly better, with AUCs in the 60–70% range, but still fails to fully account for the complexity of polygenic diseases.
The OmicsEdge PRS Model demonstrates a significant improvement, with AUCs ranging from 70% to 85%. By incorporating thousands to millions of variants, this approach captures a more comprehensive picture of genetic risk, providing good to very good discrimination across all tested diseases.
The OmicsEdge Full Model, which integrates non-genetic factors alongside the PRS, achieves AUCs from 80% to over 90%, with type 1 diabetes exceeding 90%. This combination of genetic and clinical data creates a 360-degree risk assessment, pushing discrimination into a range rarely seen in diagnostic testing.
Two main factors explain why these advanced models outperform simpler approaches. First, capturing the polygenic complexity of disease is essential. Most diseases are influenced by thousands of genetic variants, each contributing a small amount to overall risk. Focusing on a single SNP or a limited number of GWAS hits misses the majority of this signal.
Second, holistic integration with additional risk factors improves predictive accuracy. By considering demographic, clinical, and lifestyle information alongside genetics, full models provide a much richer and more reliable assessment of disease risk, offering very good to excellent discrimination across multiple conditions.
Real-World Implications for Personalized Health
Accurate genetic risk prediction can make a real difference in personalized health. OmicsEdge has developed advanced Polygenic Risk Score (PRS) models that look at many genetic factors at once.
These models can help identify people at higher risk for certain diseases, which can guide prevention, lifestyle changes, and medical decisions. Reliable risk information helps people make informed choices instead of guessing.
SelfDecode, powered by OmicsEdge, brings advanced PRS directly to consumers, while PromicsEdge provides professionals with deeper tools to use in clinical and research settings.
Models that use only one SNP or a few GWAS-identified variants often don’t provide accurate predictions. They capture only a small part of the genetic picture, which can be misleading. People may overestimate the importance of a single variant, causing unnecessary worry or giving a false sense of security. Different platforms may even give conflicting results, adding to the confusion.
Advanced PRS, like those from OmicsEdge, combine thousands to millions of genetic variants. This approach gives a much clearer view of disease risk. It allows for better risk stratification, meaning people can be grouped more accurately by their real risk. With this information, recommendations for lifestyle, monitoring, or prevention can be more targeted and useful.
Validation studies are important for confidence in any model. OmicsEdge’s PRS has been tested on large, independent datasets, showing it provides reliable predictions. Combining genetic data with age, sex, ancestry, and other clinical factors makes the risk assessment even stronger, giving a more complete picture than simpler methods.
The Bottom Line
Building advanced PRS models like OmicsEdge’s takes time, data, and resources, but the results are far more accurate than simpler methods. Single-SNP or GWAS-only models are cheaper and easier, but they often don’t give meaningful predictions.
For personalized health decisions, like prevention, lifestyle changes, or clinical planning, using validated PRS combined with clinical and demographic data is the best approach. This method provides reliable, actionable insights that are much more useful than looking at just a few genetic variants.
For individuals, platforms like SelfDecode, powered by OmicsEdge, offer actionable insights. For professionals, PromicsEdge brings validated PRS into clinical workflows. For health-tech companies, OmicsEdge provides custom PRS services and integration solutions.