Taking probiotics can help give your microbiome a little boost – it can help you strengthen the good bacteria in your gut. This may be especially important if you have IBS. But how does it work, and how can your genetics play a role in gut health? Read on to learn more about probiotics and IBS.
Introduction To Probiotics And IBS
There is this place, this world as it were, that is home to trillions of organisms that all live and work together to try and ensure that the world is a safe and healthy place. That world is you. The organisms are the microbiota of your gut, hundreds of species whose job it is to help keep you healthy.
If you put the genome of your gut’s microbiome together, it would exceed your own more than 100 times over [1]. There’s a lot of stuff living in there. Your microbiome can get out of balance though, affected by your environment, stress, what you eat, your own genetics, and so forth.
So, if you’re struggling with gut issues, it makes sense to add a few new colonies to your world, especially in the case of a condition like irritable bowel syndrome, where your microbiome may not be helping out as it could be.
This is where probiotics comes in. So, let’s explore more about probiotics and IBS, and see how that might help.
Some Facts About IBS
IBS stands for Irritable Bowel Syndrome. It is what doctors call a functional gastrointestinal disorder, which basically means that your brain and your gut aren’t communicating on the best of terms.
It is marked by abdominal pain, bloating, constipation and/or diarrhea, and is classified by whether your stool is hard, watery, or a mix [2]. It’s classified in this manner for medication purposes.
It’s not an uncommon condition. Somewhere upwards of 20% of adults in the U.S. have IBS symptoms, but less than half of that get diagnosed [3]. Depending on the severity and regularity of the symptoms, and it varies a lot, it might affect some more than others. Because of this, many people may not consider what they have to be a chronic condition.
You’re more likely to get it if you are under 50, female, have or had mental health issues like anxiety or depression, or have a family history of the condition [4].
The precise cause of IBS isn’t known, but the following appears to play a role [4]:
- Muscle contractions in the intestine (cramping)
- Nervous system (overly sensitive to intestinal pain)
- Severe gut-related infection
- Stress and/or stressful events, especially if from childhood
- Differences in gut microbes
There is no known cure for IBS, but there are steps you can take to help soothe your gut. Taking probiotics for IBS, for example, may be able to help you bring order to your microbiome.
The major instigators of symptoms seem to be stress and/or food, which is part of the reason why it goes undiagnosed so often. Stress and diet are variable factors, which can make it difficult to pinpoint an issue.
We’re going to focus on the food part of this equation here, particularly that “changes in gut microbes” part. This is where probiotics are going to come into the picture.
What Are Probiotics?
When you are born, and over the course of your first year of life, your gut is colonized by millions of microorganisms. You get some of this from your mother, but the rest comes from the environment, creating your own unique, microbiome [5].
This microbiome, full of bacteria, fungi, virus, and protozoa, are a multi-trillion “man” army involved in metabolic, nutritional, physiological, and immunological processes [6]. When your microbiome is balanced, it can help keep you healthy.
Your microbiome is integral to the connection between your gut and your brain, and may even affect mood and brain functioning [1]. [5].
But these microorganisms are not fixed at birth. What you eat can have an effect on your microbiome. People around the world have different bacterial profiles because of differing diets [7].
You can add to that biome with probiotics or interfere with it by consuming poor dietary choices like bad fats, sugars (natural and artificial), processed and fried foods. These poor choices can compromise your army and make you more susceptible to a number of problems like immune disorders and insulin resistance [6].
You can help compensate for some of these bad dietary choices by consuming probiotic-rich foods. Probiotics occur in fermented food products such as yogurt, kefir, sauerkraut, cabbage kimchi, and soybean-based miso and natto [5].
Let’s dig into some more specifics of probiotics related to IBS.
What Are The Benefits Of Probiotics?
When it comes to gut health, “balance” is the key word. For the sake of argument (because we know everything is interconnected), let’s say you have this whole stress thing figured out. We’ll take that off of the table and assume that the problem of IBS is entirely gut-related. In this case, what matters is your microbiome and what you are putting into it.
You can make sure your diet is richer in probiotic foods, but understand that they are mostly fermented. This may not suit some people, and these foods don’t have all of the useful microorganisms you’d want to consume. So, you might want to consider probiotic supplements to receive a fuller regimen of probiotics.
What will they do for you? How can you choose the best probiotic for IBS, if there is such a thing? IBS may cause a reduction in intestinal Lactobacilli and Bifidobacteria [8], which may make these a good choice of probiotics.
In general, though, probiotics may improve IBS symptoms. Some of the ways probiotics may do this include:
- Decreasing the number of potentially bad microorganisms and pathogens, and making you less gassy and more regular [9, 10, 11, 12, 13].
- Improving the composition of the microbiome [14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26]
- Preventing multiple types of diarrhea [27, 28, 29, 30, 31, 32]
- Relieving constipation [33, 34, 35, 36, 37, 38]
- Relieving the symptoms of IBS [39, 40, 9, 41, 42]
- Strengthening the gut barrier [43]
It should be noted that while all of these are beneficial outcomes, the research does seem to support differences in effectiveness for probiotics for men and women [44].
There are many other ways how probiotics can benefit your gut health. But now we must consider genetics. How can and does your DNA fit into this picture?
Your Genetics And IBS
One of the primary sources of IBS issues is inflammation. Two proteins involved in this that have been researched are TNFSF15 and IL-10. The first is a pro-inflammatory signaler in our immune response, while the other is an anti-inflammatory signaler.
In a balanced system, IL-10 will counter TNFSF15. Genetic mutations, however, can skew this system for better or worse.
For example, the SNP rs4263839 TNFSF15 raises its signaling power such that anti-inflammatory responders can’t compensate. This can create an inflamed state for your gut, which may promote IBS.
Conversely, the IL-10 rs1800896 GG genotype makes it produce at a higher level, so it’s better able to counter a TNF signal [45]. This lowers your risk for IBS.
Are these the only genes affecting your risk? No, there are others. Remember that stress is heavily involved in IBS, and there are a lot of genes related to your stress response. The fact is, with any system in your body, things are interconnected in ways that make it difficult to tell how much influence is coming from where.
Your goal should be to take specific information like what we presented here, combine it with other specific information about your genetics, and develop a plan for lowering your risks across the board.
For example, if you’re more prone to responding strongly to stress, that’s an area you might want to focus on in order to optimize your gut health. Analyze your strong and weak points and adjust your lifestyle, nutrition, and exercise accordingly.
Are Probiotics A Good Strategy Handling Your IBS Risks?
You can find many strategies to help soothe your gut, but what works for someone else might not work for you. Do probiotics for IBS work? If you have the TNFSF15 mutation then utilizing probiotics may be beneficial for you.
But remember, your health is complex, so it’s important not to take this advice in isolation. Remember that inflammation is only part of the IBS equation.
There are other elements like stress that can play a huge role in your gut health. An example would be a mutation in your COMT gene that makes you more sensitive to stressors, and part of IBS is an over-sensitivity to what is going on in your gut.
The fact is, not only do genetics influence your risks for experiencing gut problems, but it also affects how well you respond to strategies to help you address your genetic predispositions. Understanding your genes may give you an advantage when learning where to focus to achieve optimal gut health.
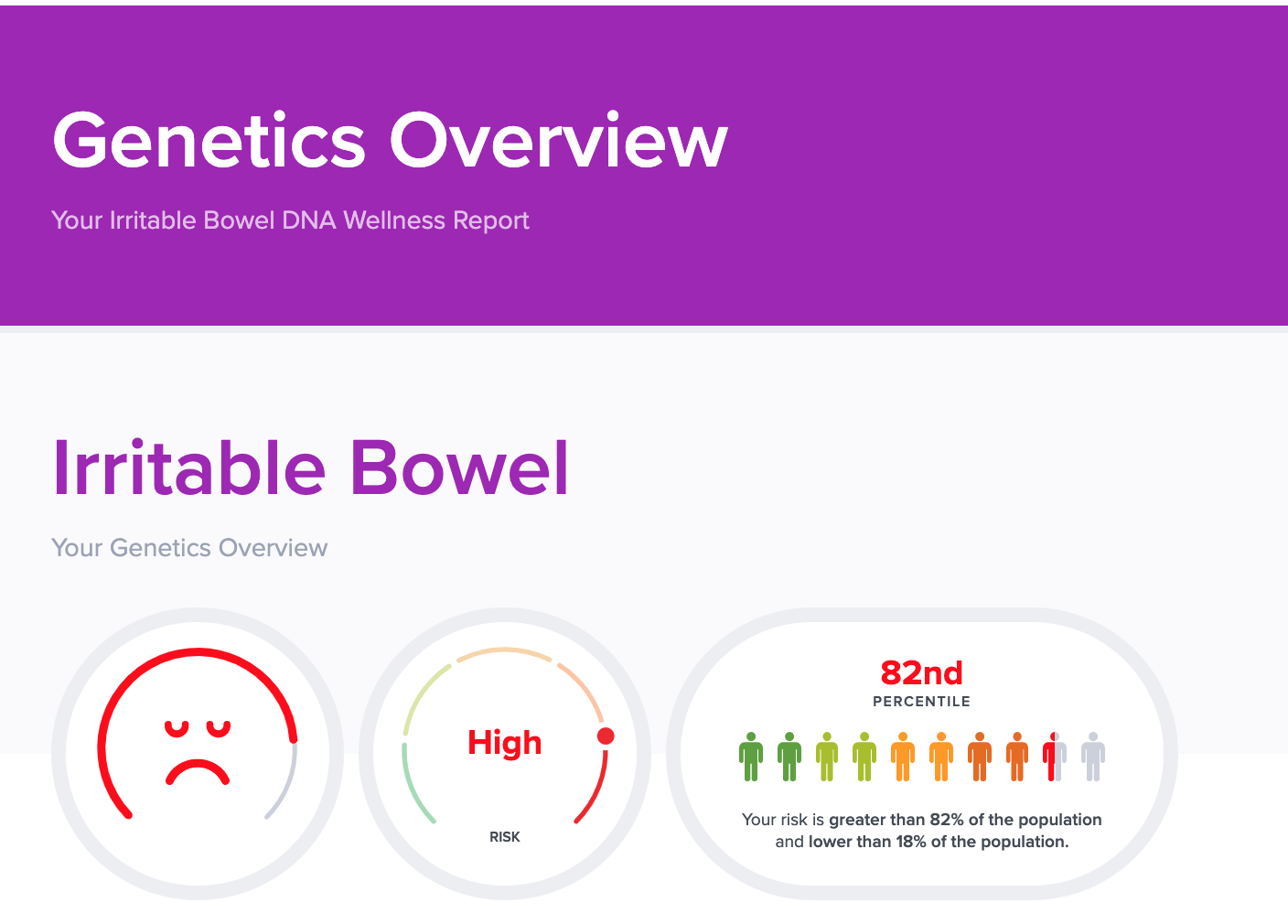
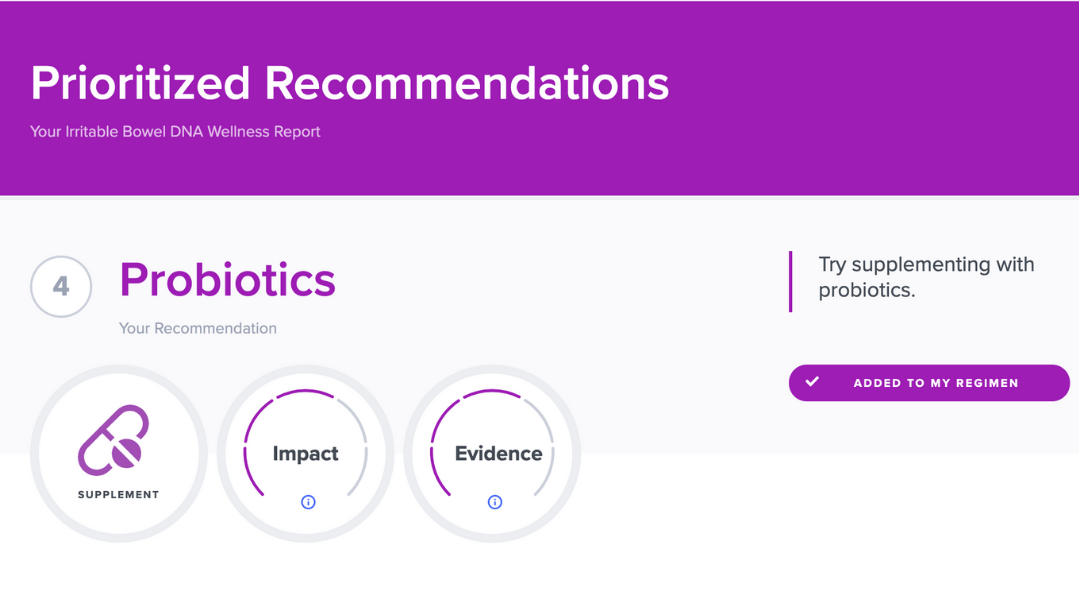
If you’re interested in a gene-based approach to improve your gut issues, you should check out SelfDecode. Unlike other DNA companies that only analyze a handful of genetic variants, the SelfDecode Irritable Bowel DNA Report looks at over 390,000 variants to give you the most accurate and science-backed results.
Not only that, but SelfDecode also provides you with a prioritized and personalized list of recommendations based on your DNA to help you optimize your gut health. You can easily add these to your regimen and implement them to best fit your wellness routines.
The strategies that work best for you may be written in your DNA, and SelfDecode can help you discover them! Plus, by signing up for SelfDecode, you’ll get access to this and 20+ other DNA wellness reports, including gut inflammation and stress.
Concluding Remarks About Probiotics For IBS
Before you go off to buy probiotics for IBS, there are a few things to consider. As discussed, inflammation and stress are some of the things that can play a role in your gut health. It’s important to understand what factors are contributing to your gut issues so you can address them head-on.
Your genetics can influence your risks for gut issues and how well you respond to gut-soothing strategies. If you want to find out what your genes have to say about your gut, check out SelfDecode.
Related Articles
- Is IBS Genetic? Types, Risks & How To Deal
- Peppermint Oil And IBS: What You Need To Know
- What Does Lactose Intolerance Feel Like?